|
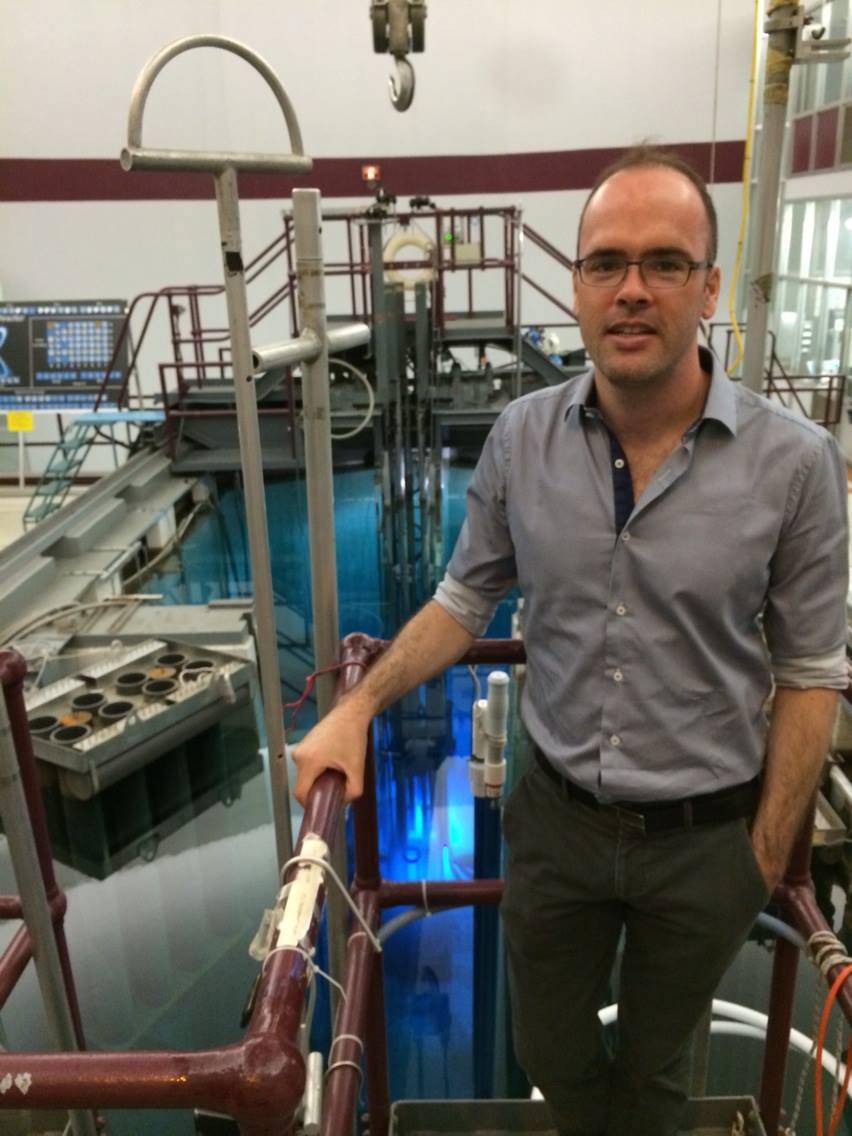
Medical Physicist
McGill University Health Centre
Assistant Professor
Department of Oncology,
McGill University
Associate member
Medical Physics Unit, McGill University
Department of Physics, McGill University
Department of Biomedical Engineering, McGill University
Medical Physics Unit
Cedars Cancer Centre, DS1.7141
1001 boul Décarie
Montréal, Québec
H4A 3J1
Canada
john.kildea at mcgill.ca
514 934-1934 ex 44154
|
Quick Links
- Research
- Teaching
- Notable software projects
- Opal
(Oncology patient application)
- Depdocs
(Documentation sharing and management for healthcare
institutions)
- SaILS
(Safety and Incident Learning System)
- Conferences
|
Clinical Work
My clinical medical physics duties
include radiotherapy treatment support,
treatment plan quality control, brachytherapy
treatment planning and quality assurance of
radiotherapy equipment. I also lead the risk
management committee in radiation oncology at
the MUHC, perform certain radiation safety
duties as part of the Medical Physics radiation
safety committee, and lead various software
projects for the Cedars Cancer Centre.
When I learn new things in the clinic I write
them down so that I don't forget. You can find
my clinical notes here.
Clinical Training and Certification
On completion of my M.Sc in medical
physics in February 2010, I undertook a two-year
on-the-job residency
training at the McGill University Health
Centre. In 2012 I passed
the membership exam of the Canadian College
of Physicists in Medicine.
Clinical Software Support
In addition to my day-to-day clinical
duties, I provide significant software support
for the Division of Radiation Oncology at the
Cedars Cancer Centre. This varies from
developing and maintaining database query
reports for the clinical team (currently over
100 such reports are in use) to developing major
software projects to support patients and staff.
Examples include a document management suite for
healthcare institutions (Depdocs), a
waiting room management software system (WORMS) and an
interface to automatically send documents
between two different clinical information
systems (ATS).
My software projects often fall into the
category of translational research; they involve
new and innovative algorithms that aim to
improve radiation oncology practice. For more
details on my various software projects please
see my software page.
Quality, Patient Safety and Risk Management
Treatment quality and patient safety are
major preoccupations in medical physics and
radiation oncology, as they are and should be in
all areas of medicine. Over the past five years,
patient safety in radiation oncology reached a
new level of urgency as a number of major
radiotherapy accidents were highlighted in the
popular press (see for example this New
York Times article). Following from the
publicity, a number of major initiatives were
developed worldwide to learn from errors so to
prevent their recurrence. In Canada, the Canadian
Partnership for Quality Radiotherapy has
taken the lead in developing the National
System for Incident Reporting - Radiation
Treatment. The NSIR-RT system incorporates
a taxonomy of incident reporting nomenclature to
help radiation medicine professionals to report
and categorize radiotherapy incidents in a
standardized manner.
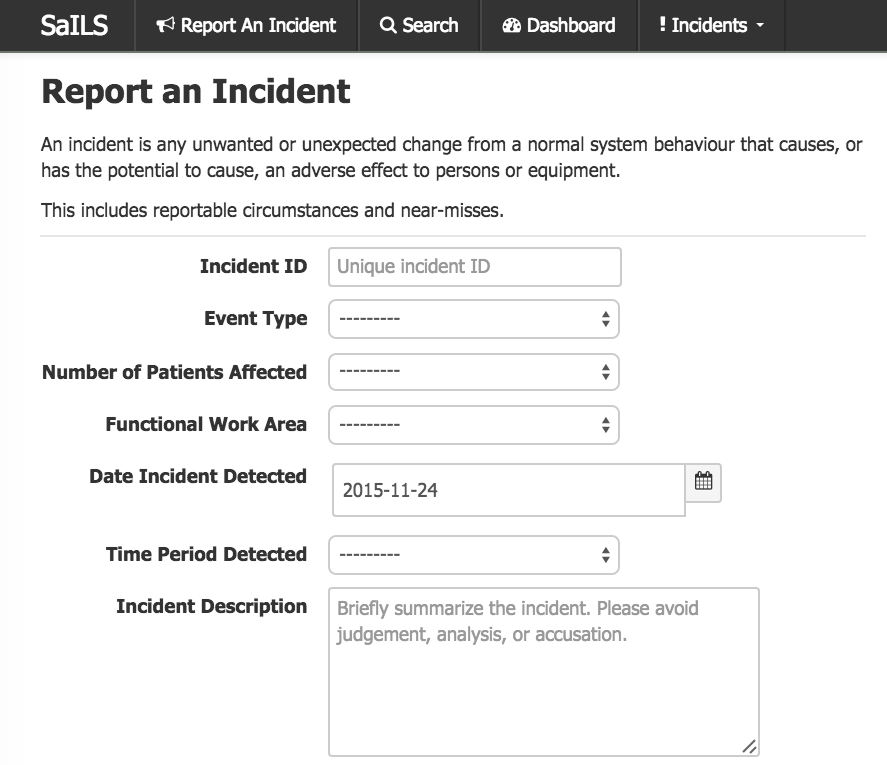
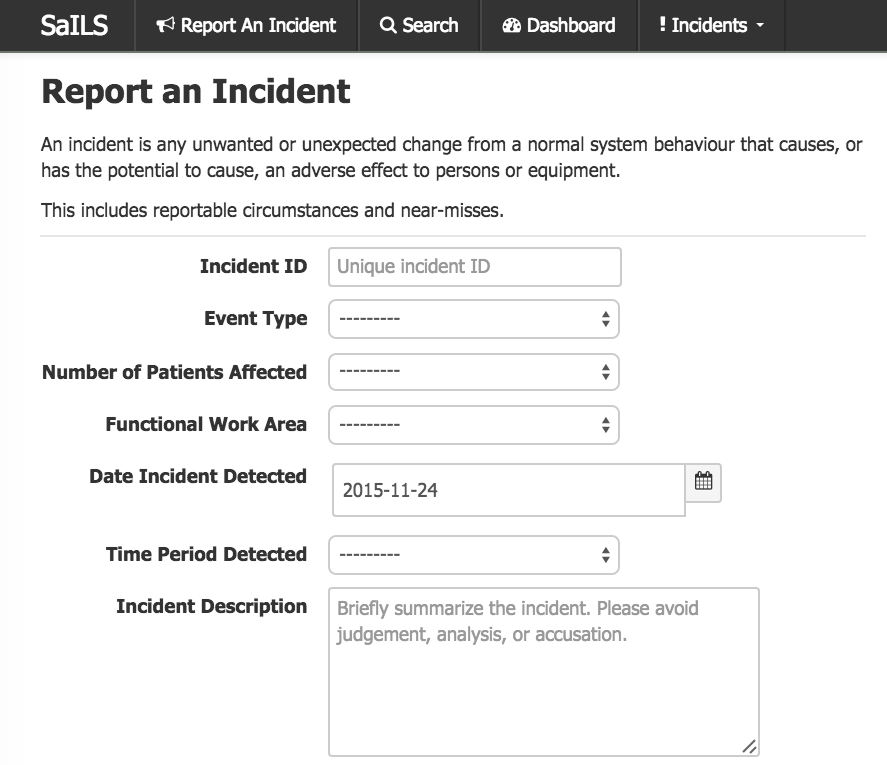
SaILS - Safety and Incident Learning System
At the MUHC I am leading an effort to implement
the NSIR-RT taxonomy into clinical practice.
With funding support from the CPQR, my graduate
student Logan Montgomery has updated the SaILS
(Safety and Incident Learning System, developed
originally by Randle Taylor at the Ottawa
Hospital Cancer Centre) to use the NSIR-RT
taxonomy. With the support of our
multi-professional risk management committee, we
are incorporating the NSIR-RT taxonomy into our
day-to-day clinical workflow. More information
on SaILS is available on my software page.
In addition to SaILS, I proposed and developed a
software tool to automatically audit patient
electronic charts in radiation oncology at the
MUHC to search for patient records that stand
out as different from the norm. Each patient is
unique but in a database of thousands of
patients there are many clusters of similar
patients. Similar patients with similar diseases
should receive similar treatments. If they do
not, something may be amiss with the
prescription or treatment plan. Our software
tool, called AEHRA (automated electronic health
record auditing) is designed to run nightly on
the electronic medical record database and flag
patient treatments that stand out from the norm
for their cohort. Initial funding for this
ongoing project was provided by the Canadian
Patient Safety Institute. Our technical
report on the project can be found here.
More information on AEHRA is provided on my software page.
Patient Partnership
I am a strong advocate for full patient
participation in their own treatments and in
hospital decision-making committees. Patients
themselves know best how they feel, they are
best placed to report their own outcomes, and
they gain valuable experience during their
treatments that can inform the treating team,
hospital committees and future patients. My
interest in patient participation has come from
my experience working with a patient researcher
as a full and equal partner in the Health
Informatics Group and from the Canadian
Winter School in Quality and Safety in
Radiation Oncology that I directed (2015
and 2016). At the 2015 Winter School in Kelowna,
BC, keynote speaker Jan Davies and patient
researcher Laurie Hendren were both very clear
that patients should be full partners in their
treatments. Please see the article I wrote about
Laurie's presentation here.
It might seem unlikely at first sight but
patients have a lot to offer the field of
medical physics. Patient-reported outcomes,
coupled with aggregated dosimetric data offer
great potential for evidence-based improvements
in radiation oncology outcomes. The Oncospace
project at Johns Hopkins is a excellent example
of what can be achieved. Medical physicists too
have a lot to offer patients. We understand and
we can explain to patients and family members
how radiation is produced and how it interacts
with tissue. We often underestimate the
usefulness of our knowledge and our role in
reassuring patients that their treatments are
safe. The
UCLA medical physics team letter to patients is
a nice example of direct communication with
patients.
 Radiotherapy patient education booklet
Radiotherapy patient education booklet
|
|